Health Planning
Health Priorities
Health planning is a Gippsland PHN core function. Knowledge about the needs of the Gippsland population is integrated across the organisation and influences our commissioning and activities.
A particular focus is on vulnerable groups such as people with mental health and alcohol and other drug issues, Aboriginal and Torres Strait Islander people, people with a disability, children and young people, older people and people with social and financial worries.
Resources
To achieve our vision of a measurably healthier Gippsland, we work in partnership with other organisations that have a health planning role. These include our six local governments as partners in municipal public health and wellbeing planning. A shared understanding of population health needs based on data and local information and agreed outcomes is a good foundation for progress towards improved health.
During 2017/18, Gippsland PHN published new resources to help stakeholders find relevant information about the health of Gippsland people.
They can be found via the Gippsland PHN website — https://www.gphn.org.au/populationhealthplanning/resources-2/
Local Government Area (LGA)
Health Needs Snapshots 2018
These one-page snapshots are designed to raise awareness of health needs in local areas and to inform conversations about how to best address the needs. Three of six LGA Snapshots include the shire's logo, highlighting the partnership approach.
Gippsland PHN staff have shared these snapshots when engaging with stakeholders. More than 200 have been used in some LGAs, indicating wide distribution.
Population Health Planning Hub
This is a downloadable Excel spreadsheet with more than 300 indicators for Gippsland and its LGAs. It can be filtered to show information for a specific health issue and/or population group and provides a reference to the data source for interested users.
Health Issue Fact Sheets
These fact sheets will be published by the end of 2018.
They will provide a one-page regional overview of each priority health issue.




Population health planning
Needs and Analysis
Gippsland PHN works to learn more about health needs by talking to people in Gippsland. We use this knowledge alongside other data and information to understand health and wellbeing needs for the region and for local areas. Our knowledge about what is most needed informs the organisation and influences our commissioning and activities.
Consumers and Carers –
Mental Health and Alcohol and Other Drugs
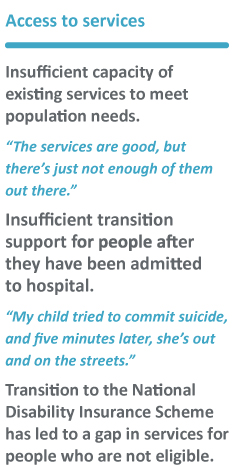
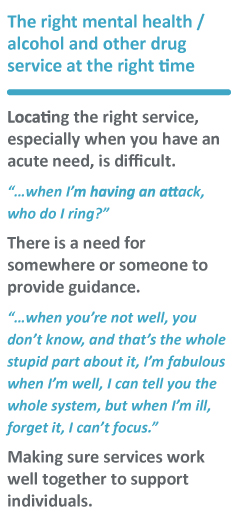
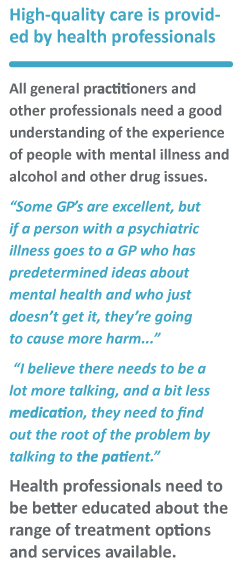
In 2017/18, Gippsland PHN held three focus groups with consumers and carers who had accessed mental health and alcohol and other drug services in the region. They reported a range of experiences including the availability and the quality of each service that they had access to. Overall, the feedback suggested that their individual needs were not effectively met. Good-quality care was dependent on finding an individual health professional who would listen to them and who was sufficiently knowledgeable and skilled.
Some priorities identified by this group include:
Consumers and Carers – Older people
Gippsland PHN worked with the Health Issues Centre to learn more about the needs of older people. Social media, surveys and interviews were used to learn from older people, their carers and health professionals.
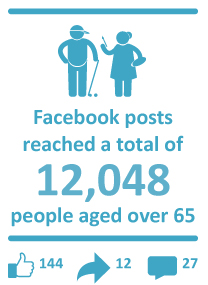


Information from these conversations highlights the critical importance of the older person’s identity and social inclusion for healthy ageing. From a health service perspective, it shows the importance of clinical empathy and effective communication as an opportunity to keep older people engaged with clinical services. Some findings from the research:
LOSS OF CAPACITY AND INCREMENTAL DECLINE The loss of both physical and cognitive capacity was a major concern for people aged over 65 years. Many people indicated the impact their declining health and capacity had on their personal identity and emotional wellbeing.
“I can no longer take a holiday, or go and visit my family, I can’t even see a movie any more ...” (Ageing person)
IDENTITY A number of people indicated a struggle to maintain their own identity as they aged. This was commonly linked to the realisation of their diminishing physical and mental capacity. Negative interactions with health services and other environments exacerbated this problem.
EMPATHY AND VALIDATION Many respondents reported negative personal experiences where they believed they had been patronised or treated as unreliable witnesses to their own lived experience. Health and social service providers’ inability to demonstrate empathy and validation was a key barrier to health and social care.
"Some health professionals just don’t want to listen. You’re just there for a reason and let’s deal with that and they don’t want to listen past what your complaint is." (Ageing person)
COMMUNICATION OF CLINICAL INFORMATION A number of consumers, including those diagnosed with dementia as well as those with high cognitive function, were concerned about doctors not taking the time to explain their diagnoses, reasons for treatments and treatment instructions.
GENDER In some instances, the ‘traditional’ role older women undertake as the nominated carer of family members and ‘housewife’ responsible for upkeep of the home extends to their responsibility to access home care and health services for themselves and on behalf of their partners.
ACCESS LOGISTICS A number of logistical barriers were frequently identified as major inhibitors to accessing health and social care services in rural areas. These barriers included: long waiting times for GP and other clinical appointments; cost of services and travel; distance and transport to and from services; reduced access to technology including phones and internet; and dependence on temporary accommodation nearby to services.
"...it is the access, and inconvenience, that creates the stress. People are kind, but generally, specialists are completely ignorant of the rural situation, and the inconvenience some of their recommendations and appointments have." (Ageing person)
CARER SUPPORT Responses from adult children of ageing parents highlighted the burden of responsibility on families to provide care for people in advanced stages of health decline and dependency.
"I’m so tired. I waited over 12 months for a carer's pension to be approved and although I did receive back pay it put tremendous strain on my marriage, which still hasn’t recovered." (Adult child of ageing parent, carer)
HealthPathways Gippsland
HealthPathways Gippsland launched in February 2017 and has continued to evolve as a useful resource for Gippsland health professionals, providing best practice clinical guidance in a local context for many conditions.
These conditions are supported by local referral pathways, enabling GPs and other health professionals to make informed decisions on the best way to connect their patients to the right care, at the right place, at the right time.
HealthPathways Gippsland brings together GPs, specialists, nurses and allied health professionals to contribute to local pathway development guiding best practice assessment of a range of medical conditions, including when and where to refer patients.
HealthPathways Gippsland has been promoted and demonstrated at the following events:
- GPCE Conference
- I.CAN working group meeting
- Gippsland Allied Health Symposium
- GRICS Prostate Cancer Conference
- Victorian Rural Health Conference
- LRH Telehealth Project Steering Group
- GPHN-led training events.
In addition to engaging with GPs, our local subject matter experts consist of the following health professionals:
- paediatrician
- ophthalmologist
- pharmacist
- gastroenterologist
- respiratory physician
- pharmacotherapy
- psychiatrist
- pain specialist
- haematologist
- palliative care
- family violence.
What’s Next for HealthPathways Gippsland?
The HealthPathways team will continue to collaborate with local GPs, specialists, nurses and allied health professionals to actively encourage in local pathway development.
The pathways in development include:
- paediatric pathways for allergy, ENT and neurology
- diabetes
- asthma
- cardiovascular disease
- older persons health including dementia
- behavioural and developmental concerns in children
- IV iron infusion.
Program Highlights




Participation agreements with 10 health services within Gippsland (including hospitals)
- West Gippsland Healthcare Group
- Bairnsdale Regional Health
- Bass Coast Health
- South Gippsland Hospital
- Orbost Regional Health
- Yarram District Health Service
- Latrobe Regional Hospital
- Central Gippsland Health Service
- Gippsland Lakes Community Health
- Latrobe Community Health Service


Pictured (L-R): Roman Zwolak — RWAV, Shae Wissell — RWAV, Marianne Shearer — CEO GPHN, Jeannette Douglas — HealthPathways GPHN, Megan Cahill — RWAV, Christine Fishley — Murray PHN, Michelle Hearn — HealthPathways Grampians Ballarat, Cara Miller — HealthPathways Horsham Wimmera.



Commissioning
In 2017/18, Gippsland PHN has demonstrated increased PHN systems sophistication and significant improvement in monitoring quality and measuring service performance, including increased community access to care. This has taken assertive training and education for PHN staff, implementation of accountable contracts, as well as building capability, motivation and incentives for providers.
In 2017 the cumulative aggregated commissioned services access achievement was 17,061 occasions of service compared 47,179 in 2018, more than 177% increased access to services for the community this year and greater productivity for almost the same investment.
2017/18, services were commissioned across 12 program areas through 53 contracts. Within several of the program areas different service streams exist.
Commissioning Highlights
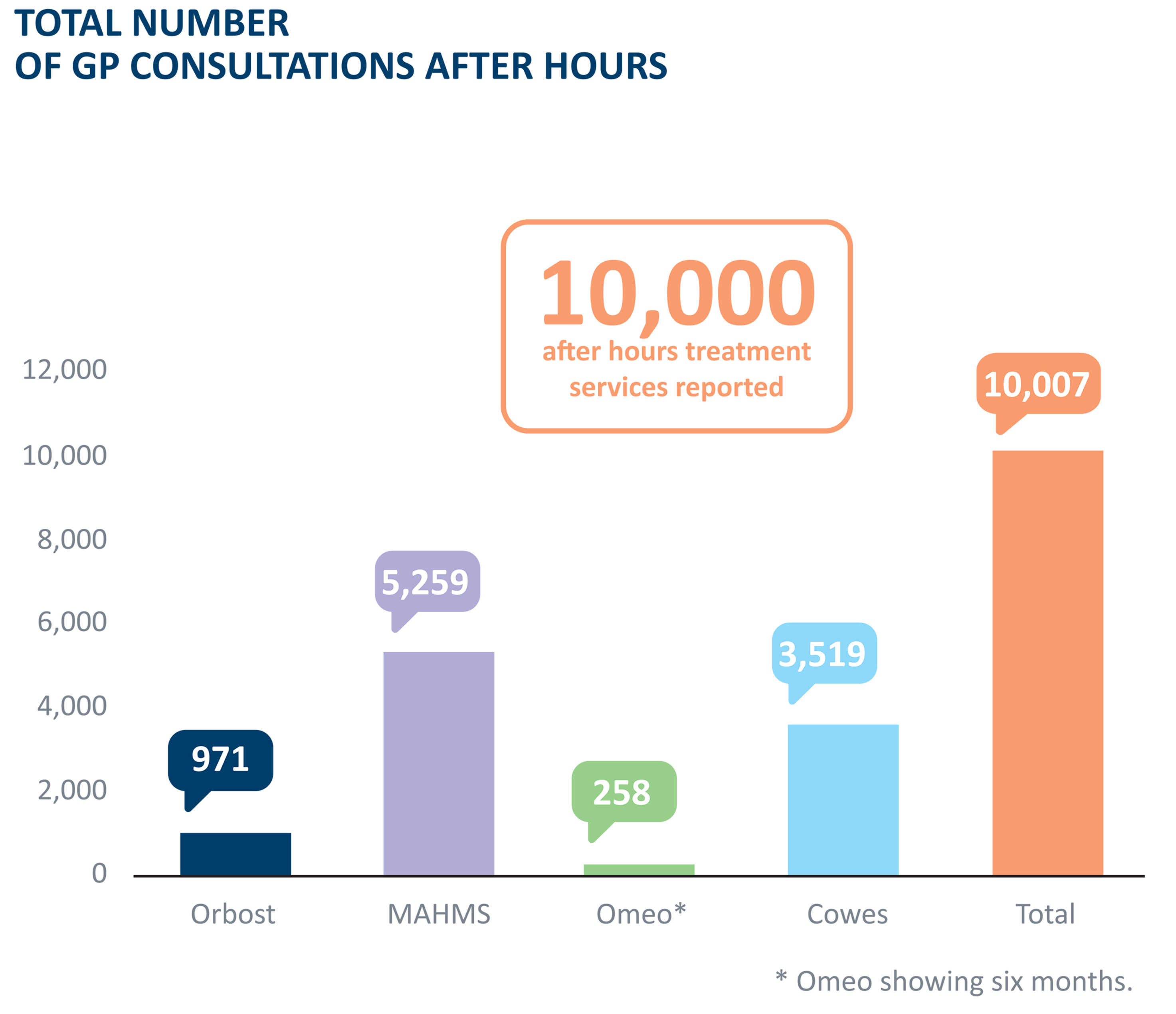
- After-hours care reported more than 10,000 treatment services
- Place-based flexible funding delivered 16,600 treatment and health promotion services to remote communities with a particular focus on chronic disease management and early intervention.
- Aboriginal and Community Controlled Health Organisations were delighted to report more than 2,700 care coordination and outreach services to their Indigenous communities.
- Mental health and drug and alcohol services are commissioned in many settings across Gippsland, and together delivered more than 20,000 services. These services are now co-designing the mental health stepped care model, aiming for full-roll out and flexibility for 2018/19.
- New services include nine settings established for doctors in secondary schools, funded by the Department of Education and delivered by local general practices.
- The four Youth Assist Clinics expanded in Gippsland South Coast, using PHN funding to prepare for the transition to the imminent hub and spoke integrated headspace model. Headspace Bairnsdale launched and ramped up its presence and community outreach in its first year.
- The Innovation Grants were highly successful, awarding 10 small grants and establishing an online Ideas Bank to progressively develop novel and 'shovel-ready' projects for new opportunities of interest to community and health providers.

Mental Health
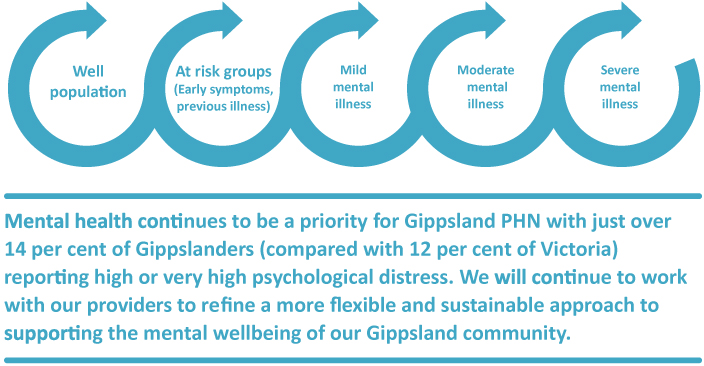
Stepped Care Approach to Mental Health
Stepped care is an evidence-based, staged system comprising a hierarchy of interventions, from the least to the most intensive, matched to the individual’s needs.
While there are multiple levels within a stepped care approach, they do not operate in silos or as one-directional steps, but rather offer a spectrum of service interventions.
Gippsland PHN has worked with the sector through the Mental Health Reform Project and other commissioning activity and commenced delivery of the stepped care approach.
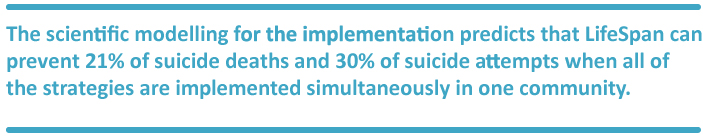
Place Based Suicide Prevention Trials
The Place Based Suicide Prevention Program is funded jointly by the Victorian Department of Health and Human Services and Gippsland PHN to work with communities, including the wider population, health agencies, local governments, emergency services, schools and media outlets, to contribute to the reduction of the suicide rate within the Latrobe Valley and Bass Coast Local Government Areas.
The place-based suicide prevention trials aim to apply the LifeSpan Model of suicide prevention to:
- reduce rates of suicide
- reduce suicide attempts
- improve individual resilience and wellbeing
- improve the system to prevent suicide in an ongoing way.

Youth and Child
Youth and Child (headspace)
In 2018, Gippsland PHN commissioned Relationships Australia Victoria (RAV) to lead the new headspace services in Bass Coast and South Gippsland. The new services will be established as a centre (based in Wonthaggi) and outpost model, incorporating and supporting four existing Youth Access Clinics in Foster, Leongatha, Korumburra and Wonthaggi and adding a fifth site on Phillip Island to provide an efficient, effective and integrated approach across Bass Coast and South Gippsland.

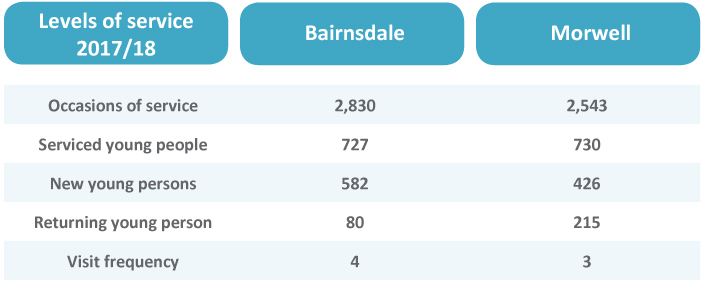
Youth Access Clinics
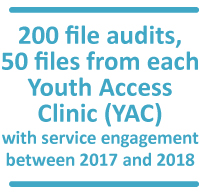
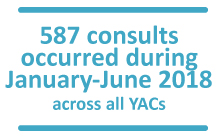
Orygen was funded to conduct two research studies of the Bass Coast and South Gippsland Youth Clinics. One study was a file audit and the other a qualitative study of stakeholders, including young people attending the clinics.
Descriptive statistics were used to analyse the data and identify themes.
The results showed that young people presenting for care to the YAC clinics in Gippsland:
- are young, with a mean age of 16 years
- present with high levels of self-harm, mental ill-health, suicidal ideation, family conflict, exposure to trauma, and alcohol and substance misuse
- engage in sexual behaviours at a young age
- are witness to, or experience, interpersonal violence
- are experiencing or are part of families that are experiencing financial struggles
- come from a variety of living situations with a large number of single parent families
- are less likely to be males.

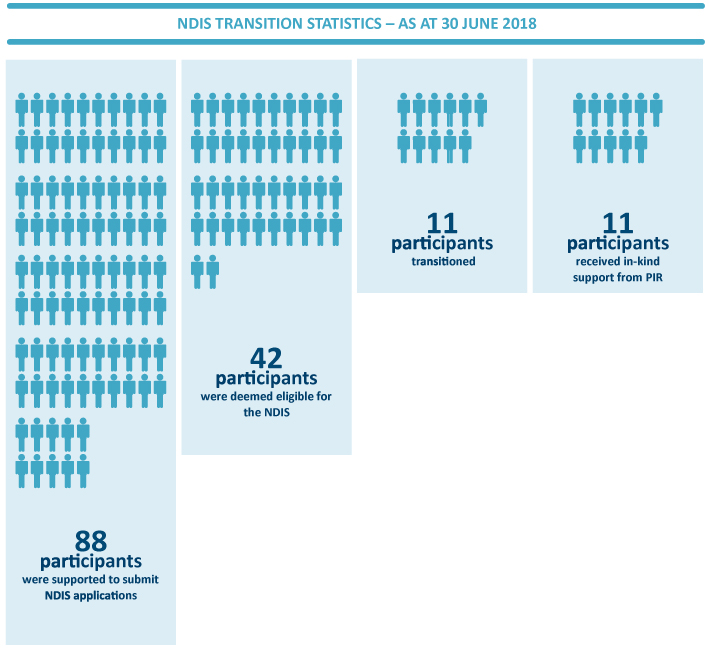
Partners in Recovery Program
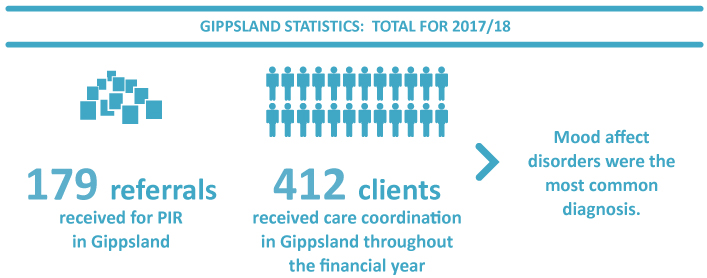
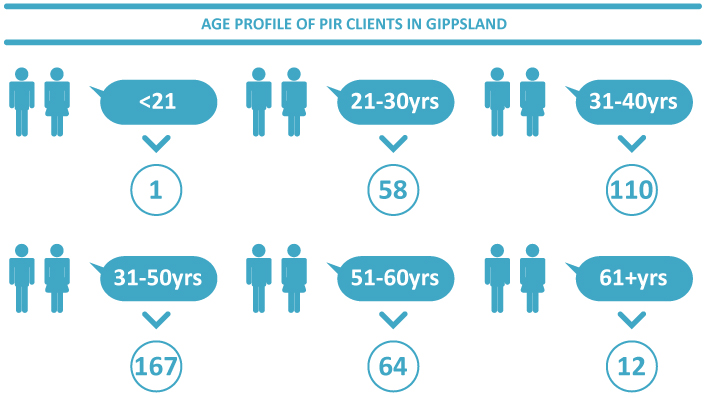
Partners in Recovery (PIR), an Australian Government initiative, is delivered on behalf of Gippsland PHN by Wellways and Mind Australia, and is accessed via central intake provider the Australian Community Support Organisation (ACSO).
The programs work to improve the systemic response to the needs of adults with severe and persistent mental illness with complex needs, and their carers and families.
Since the National Disability Insurance Scheme (NDIS) has been introduced, it is expected 97 percent of PIR participants will transition to it. In addition to delivering the program, our PIR organisations are helping clients to test for eligibility for NDIS, supporting transition and delivering in-kind services as a component of participants’ plans.
National Disability Insurance Scheme (NDIS)
The NDIS is the new way of providing disability support. The NDIS will provide Australians under the age of 65 who have a permanent and significant disability with the reasonable and necessary supports they need to live an ordinary life. As an insurance scheme, the NDIS takes a lifetime approach, investing in people with disability early to improve their outcomes later in life.
Inner Gippsland (Latrobe, Baw Baw, South Gippsland, Bass Coast) commenced roll-out on 1 October 2017.
Outer Gippsland (Wellington and East Gippsland) is planned to commence roll-out on 1 January 2019.
Other Mental Health Services
Gippsland PHN has invested in several local agencies to deliver perinatal mental health, trauma-focussed clinical care, aged mental health, low intensity online and services for children with autism. We look forward to working closely with these organisations to help them integrate a sustainable program that provides greater accessibility to mental health services across Gippsland.
Alcohol and Drug Support
AOD Programs
Gippsland PHN’s Alcohol and Other Drug (AOD) Programs are funded by incentives and grants through the Australian Government Department of Health (DoH). Gippsland PHN has the flexibility to commission evidence-based treatment services to meet local need, catchment priorities and fill service gaps. The aim of Alcohol and Other Drug (AOD) Programs is to reduce the harms associated with drugs and alcohol in the community and improve the overall health and wellbeing of people living in Gippsland.
In 2016 a needs analysis of Gippsland alcohol and drug supports was conducted. This assisted to identify service gaps by region, activity type and workforce needs. Youth, families and carers were identified as the areas of greatest need within specific communities.

- Australian Community Support Organisation (ACSO) delivers the Family and Carer Support Service.
- Youth Support and Advocacy Service (YSAS) delivers the Youth Outreach Service.
- Latrobe Community Health Service (LCHS) delivers the Breaking the Cycle Program.
- Central Gippsland Hospital (CGH) delivers the SMART Recovery Program.
ACSO – Family and Carer Support Service
The Family and Carer Support Service operated by the Australian Community Support Organisation offers a multifaceted model of care including brief interventions, single session family work, education and peer support groups for family, carers and significant others. It provids support to those misusing substances in the local government areas of South Gippsland, Wellington, Baw Baw, Latrobe Valley and East Gippsland (with state DHHS directly funding Bass Coast).
ASCO delivered the following:
- launched a Facebook page for the Family and Carer Support Service
- established a sibling-specific Substance Abuse Support (SAS) group
- established a men’s-specific SAS group
- extended the information and education groups to target professional stakeholders and provide in-house training and professional development
- continued to raise community awareness and education surrounding the negative impacts and stigma of AOD on families, their loved ones and the community
- tackled the subject of stigma by aiming to reduce the barrier to treatment and support that it presents to people in need
Evaluation/anecdotes
"I would like to thank you for your support when I was very stressed. You have helped me to cope with the situation, things are good with my family at the moment thanks to you”
![]()
“After having spoken to you in the morning it gave me the courage to say no and not answer the phone for the rest of the day, so thank you... I almost feel empowered. Guilty, but in control”
![]()
“I had a good cry when I got home, more from relief from the burden of blaming myself, also from the thought nothing may ever change. But it was wonderful to talk & someone was listening”
![]()
“Thank you from the bottom of my heart for all your help, support and advice”.
YSAS — Youth Outreach
The Place Based Youth Outreach Service operated by Youth Support Advisory Service (YSAS) offers brief, evidence-based treatment (early intervention) for young people misusing substances are aged 12-25 years in the local government areas of South Gippsland, Bass Coast and Wellington (with state DHHS directly funding Latrobe, Baw Baw and East Gippsland).
YSAS is a client-centred service that first responds to the young person’s self-identified highest need when entering the service.


- Over the past year YSAS supported 16 young people through a supported residential withdrawal program.
- 100% of clients received a service response from YSAS with 48 hours of initial referral.
- The Place Based Youth Outreach Service operated by Youth Support Advisory Service (YSAS) offers brief, evidence-based treatment (early intervention) for young people misusing substances are aged 12-25 years in the local government areas of South Gippsland, Bass Coast and Wellington (with state DHHS directly funding Latrobe, Baw Baw and East Gippsland).



The Place Based Flexible Funding (PBFF) Program
The Place Based Flexible Funding (PBFF) Program focuses on increasing access to a range of primary and allied health services and activities for rural and remote communities, particularly smaller communities, and targets identified health needs of these communities.
The PBFF Program supports health service's target priority areas and population groups not currently resourced from other government programs. Services are provided in geographic locations within Gippsland where there is evidence of high prevalence of chronic conditions, high levels of socioeconomic disadvantage and lower access to allied and other health services.
The aim of the PBFF Program is to improve the health and wellbeing of people living in Gippsland in rural and remote locations and is structured to align with Gippsland PHN’s strategic objectives.
Gippsland PHN objectives
- Improved health outcomes for people with chronic disease and those patients at risk of poor health outcomes.
- Improved coordination of care to ensure patients receive the right care in the right place at the right time.
PBFF Program objectives
- Provide and maintain access to allied health and primary care services based on the identified health needs of the community.
- Promote coordinated, multi-disciplinary, team-based approaches to the provision of integrated primary healthcare services.
- Establish and maintain effective community consultation practices for the planning, management, flexible delivery and ongoing review of the program.
- Provide and maintain access to relevant health promotion and preventative health programs and activities designed to promote health and wellbeing.
- Encourage people living in rural and remote locations in Gippsland to adopt or modify behaviours to better manage their health and wellbeing.
Primary health care services encompass active treatment, screening programs, health education on individual health risks, and more broadly, efforts to address health concerns for the entire community.
In 2017/18 contracts for delivery of Place Based Flexible Funding services were held with eight organisations:
- Bairnsdale Regional Health Service
- Bass Coast Health
- Cann Valley Bush Nursing Centre
- Central Gippsland Health Service
- Mallacoota District Health & Support Service
- Omeo District Health
- Orbost Regional Health
- Uniting (Victoria and Tasmania Limited).
A 74-year-old man diagnosed with Parkinson’s Disease, depression, hyperthyroidism and tendonitis was referred to a physiotherapist, occupational therapist, speech therapist and podiatrist by his GP. Access was arranged for occasional respite care at a nursing home and advanced care planning was discussed as part of his regular visits. After his Parkinson’s disease advanced, the patient was referred to a neurologist. The patient was able to remain in his own home for an extra four years thanks to this support.
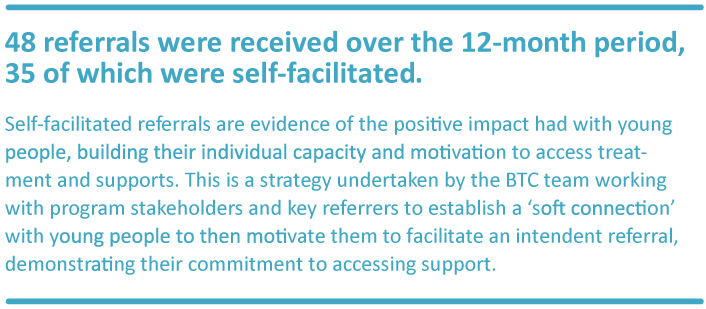
Latrobe Community Health Service — Breaking the Cycle
The Youth ‘Breaking the Cycle’ (BTC) Program operated from Latrobe City by Latrobe Community Health Service provides withdrawal linkages for young people misusing substances. A focus of this program is engaging the Aboriginal and Torres Strait Islander population, although all young people are accepted.
Latrobe Community Health Service:
- established a strong connection with Department of Health and Human Services (DHHS) Youth Justice providing opportunities for the BTC worker to be sitting out of the DHHS office and attending on court days.
- increased networking and capacity building in the Youth Justice sector and has also provided significant opportunity to engage this difficult demographic
- experienced a significant increase in ‘self-referrals’ being made to the service, which demonstrates trust and rapport established within the local community
CGH — SMART Recovery
The SMART (Self-Management and Recovery Training) Recovery is a group program assisting people with problematic behaviours, including a range of addictions, to achieve their goals. SMART Recovery commenced in Gippsland as a 12-month Innovation Project, which returned exceptionally positive feedback. Based on the program’s successes further funding has been granted to continue providing SMART Recovery in Central Gippsland (Wellington) and other locations in Gippsland.
Weekly SMART groups occur at Central Gippsland Hospital. The average group size is 8-10 people with an upward trend. The SMART Recovery group in Sale has supported people with a wide range of addiction issues, ranging from opioids, cannabis, methamphetamines, alcohol and hoarding.
Alcohol continues to be the dominant substance of addiction
Highlights
The program has provided a real opportunity to reduce vulnerability and isolation and promote community connectedness.
Program evaluation has demonstrated the positive impact in the lives of consumers and formed the evidence to support an extension of this program across Gippsland (via Bairnsdale Regional Hospital and Gippsland Southern Health Service).
Gippsland PHN’s Nilay Kocaali attended Central Gippsland Hospital (CGH) to meet four participants of the SMART Recovery group and gain direct insight into the program successes. Nilay reported was a strong element of connectedness, not only in terms of the established relationships but also extending to other primary health and support organisations. Participants shared that they had a newfound sense of hope in the wider service system, which their access to the SMART Recovery program had encouraged. Each participant concluded a significant gap would be left in their lives and the community without the SMART Recovery Program. However, they also identified the skills and developments made in relation to their mental health and coping abilities would carry forward.
Anecdotes:
“WE LAUGH things don’t seem so bad.”
“I wish I had joined a group like this before. It is good to meet people in the same situation as me.”
“I am no longer isolated and alone I feel safer.”
“The group has taught me that I am not unusual.”
“I find the group is very focused what I am able to do which is very important to me.”
Advanced Care Planning
Gippsland PHN invited general practices in January 2017 to participate in sponsored research to evaluate advanced care planning in Gippsland.
Gippsland PHN selected 10 communities and general practices from Gippsland’s six Local Government Areas where a series of interviews, involving 30 people and one general practice per community, occurred. The evaluation of advanced care planning was a collaborative approach to design, consult and gain measurable insights as to the attitudes, experiences and needs of general practitioners and their patients.
Tom Holman, Customer Focus Pty Ltd, from Foster, was appointed as the researcher and worked in collaboration with Gippsland PHN.
The objectives of the project were to:
The highly collaborative project was overseen by a reference group.
After Hours
Gippsland PHN’s After Hours Primary Health Care Program addresses gaps in after-hours service arrangements and seeks to improve service integration. The priority is to maintain existing after-hours primary care that is not within the scope of the Practice Incentive Payment (PIP) After Hours Incentive and to facilitate access to after-hours medical services through innovation and collaboration with regional stakeholders.
Key focus areas include:
- limited after-hours service across regional locations
- identifying service gaps to enhance the regional aged care services, after hours
- establishing alternative after-hours service solutions
- maintaining access to medical services in remote locations
- mitigating after-hours service gaps and increaseing consumer engagement.
In 2017/18 contracts for delivery of After Hours Primary Care Services were held with five organisations:
- Cowes Medical Group
- Omeo District Health
- Orbost Regional Health
- Mallacoota Medical Centre
- Moe After Hours Medical Service (MAHMS):
- Central Gippsland Family Practice (roster administration)
- Latrobe Community Health Service (service delivery).
Case study: Evidence of avoidable emergency department admissions
After Hours Service received a call at 19:45 from Ambulance Victoria requesting to bring elderly patient to clinic from local Aged Care facility for suturing of laceration to avoid 40min trip to nearest hospital, and a potential long wait in Emergency Department. There appeared to be no other injuries. The After Hours clinic accepted the patient for assessment and treatment. The injury was sutured and no other injuries found. Patient was able to return to the nursing home with follow up instructions and was back home in her bed in under an hour.