Indigenous Health
The Indigenous Health Program supports the health needs of Aboriginal and Torres Strait Islander people across Gippsland.
Gippsland PHN met the needs of managing chronic disease and supporting individuals affected by alcohol and other drugs and mental health barriers by commissioning two services – the Integrated Team Care Program and Dual Diagnosis Program.
Chronic Disease: Integrated Team Care
Gippsland PHN commissioned the Integrated Team Care Program (ITC) to help Aboriginal and Torres Strait Islander people with complex chronic diseases to effectively manage their conditions through
access to one-on-one assistance by Care Coordinators.
The Integrated Team Care Program consists of care coordination, supplementary services in Ramahyuck District Aboriginal Service (three sites in Sale, Morwell and Drouin,) Gippsland and East Gippsland Aboriginal Corporations (GEGAC) (one site Bairnsdale) and Lakes Entrance Aboriginal Health Association (one site Bairnsdale). Moogji Aboriginal Council East Gippsland Inc employs an Aboriginal outreach worker (non-clinical) who supports the community to attend appointments and provides community liaison and practical assistance.
Program Highlights
- Integrated Team Care Program delivered 2,761 occasions of service.
- The Indigenous Health Program is continuing to grow and achieve positive outcomes for community members, which is demonstrated by access targets being exceeded.
- Care coordinators have strong relationships with the program officer where they can seek assistance to
understand the program requirements to enable increased service delivery and quality of service. - Contract deliverables have been tailored to respond to the Indigenous population's needs with a strong understanding of culture, taking into account holistic health needs of the Indigenous community.
Drug and Alcohol: Dual Diagnosis Service
The Gippsland Indigenous Dual Diagnosis Service (IDDS) was designed to strengthen linkages within the stepped care mental health model for clients in the mild to moderate range.
This program assisted in providing culturally appropriate, evidence-based mental health and alcohol and other drugs (AOD) services for Aboriginal and Torres Strait Islander people to improve access and complement and link to existing services.
Latrobe Regional Hospital (LRH) was part of the statewide Victorian Dual Diagnosis Initiative (VDDI) and delivered the IDDS until June 2018.
Objectives
- Improve response, treatment and outcomes for Aboriginal and Torres Strait Islander people experiencing mild to moderate mental illness and drug and alcohol misuse.
- Improve response, treatment and outcomes for Aboriginal and Torres Strait Islander people with complex needs consistent with moderate to severe mental health illness, arising as a result of substance misuse.
- Increase engagement and rapport building with community members leading to reduced unplanned withdrawals from existing mental health and AOD treatment services.
- Increase awareness of mental health and AOD conditions and services for the Aboriginal and Torres Strait Islander community.
- Greater workforce capacity in the Aboriginal Community Controlled Health Organisations (ACCHOS) sector in responding and working with Aboriginal and Torres Strait Islander people who have mild to moderate mental health and AOD needs.
- Improve understanding of intergenerational trauma, discrimination, loss of land and culture, the stolen generation and its impact in the mental health and AOD sectors.
- Improve cross-sector partnerships and integration, better coordinated access and response between general practitioners, ACCHOs and mental health and/or AOD services, both clinical and non-clinical.
Program Highlights
- The IDDS employed two clinicians: One in Latrobe Valley/Wellington (Ramahyuck) and one in East Gippsland (GEGAC).
- The IDDS steering group met monthly with attendance of a community member to supply feedback from the community in Morwell. The IDDS showed growth with positive feedback received from the local Aboriginal community, which accepted the service and clinicians.
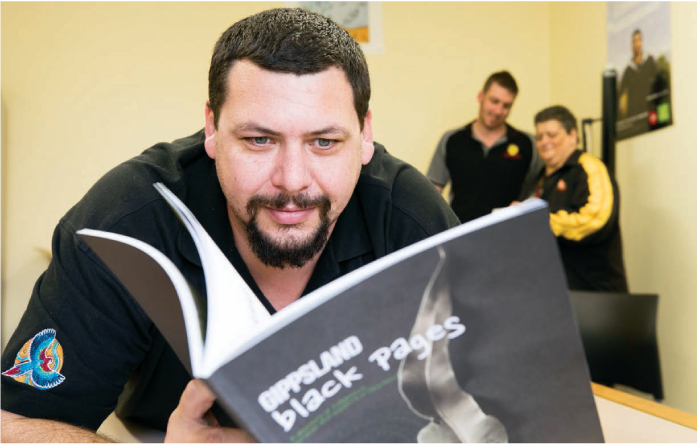
Launch of Black Pages
The Black Pages launched its online version during NAIDOC Week in July 2018. The online Black Pages assist health professionals and community members to navigate and access resources on their computers and smart phones. Hard copies of the Black Pages were printed in 2017, and distributed across Gippsland.
Opening of Dr Jane’s Place
Gippsland PHN continues to support services that genuinely engage our Aboriginal and Torres Strait Islander people to develop local, culturally appropriate strategies that identify and respond to those most at risk within our communities.
Dr Jane’s Place provides a safe place for the Indigenous community to receive healthcare within an holistic setting. A vegetable garden and a yarning room provide culturally safe areas to discuss health and life concerns and to assist with healing.

Dr Jane’s Place
Diversity in Gippsland
Gippsland PHN is committed to engaging with the community to better understand how we can support people with a diverse background and leverage from their unique experiences and perspectives.
Unique But United
Unique But United (UBU) is a program delivered by headspace in Bairnsdale. It hosts a fortnightly LGBTIQ+ support group for young people aged 12 to 25 years who want to meet other sexually and gender diverse young people and allies in a safe and supportive space.

headspace Bairnsdale has been nominated as a finalist for the 2018 Inaugural Primary Health Awards for the UBU project.